Baker-Polito Administration to Distribute $502 Million from the Federal Coronavirus Relief Fund to Local Cities and Towns
The Baker-Polito Administration today announced that it is preparing to distribute up to $502 million from the federal Coronavirus Relief Fund to local cities and towns for eligible costs related to the COVID-19 response effort. The Administration is also providing guidance to local municipalities on this formal distribution process and establishing protocols to maximize the use of federal resources and promote compliance with federal restrictions. To read more, please go to https://www.mass.gov/news/baker-polito-administration-to-distribute-502-million-from-the-federal-coronavirus-relief-fund
ARCHIVED MATERIAL
COVID-19 Outbreak Local Public Health Responds – An Open Letter from the Coalition for Local Public Health – April 17, 2020
Dear MAHB Members,
Over the last month, the Coalition for Local Public Health has been advocating tirelessly for our members, and for the broader local public health workforce. A month ago, the Coalition asked Governor Baker’s COVID-19 Command Center to invest in increasing local capacity for contact tracing. They responded by directing emergency funds to local public health departments. Subsequently, they announced directly with the Baker Administration to fine-tune the Community Tracing Collaborative. Much of our advocacy has focused on ensuring that this large-scale contact tracing initiative integrates with our local public health system and builds local capacity for the future .
We are pleased to announce that, at the request of the Coalition, the Baker Administration and Partners in Health are hosting a webinar on Tuesday, April 21 at 3pm in lieu of the DPH/LBOH call, to explain the details and timeline of the the launch of a statewide Contact Tracing Collaborative. We are pleased that they are responding to our request for investment in this area, but we recognize that there are many questions about how this new statewide initiative will impact the work of local health departments.
Recently, two representatives of the Coalition (Dawn Sibor, MA Health Officers Association and Kristina Kimani, MA Public Health Association) have been working Community Tracing Collaborative, and in order to provide clarity and detailed information to local boards of health.
As you know, contact tracing is a critical public health tool that works best when done locally. However, in this time of crisis, not all communities have the capacity to do their own contact tracing. For that reason, the statewide effort will play a crucial role. But, it must also integrate the work of those communities that do have substantial capacity and are already engaged in substantial contact tracing. By leveraging the strengths of both local and statewide efforts, we can best protect the public and save lives.
Please join us in participating in this webinar to learn how together we can leverage the Community Tracing Collaborative to stop the spread of COVID-19 and protect all residents of our Commonwealth. We will follow-up with a registration link for the webinar when it becomes available.
We are in this together,
Ruth Mori, MSN, RN President – Massachusetts Association of Public Health Nurses , Public Health Nurse, Town of Wayland
Cheryl Sbarra, Director of Policy & Law, Massachusetts Association of Health Boards
Sigalle Reiss, President, Massachusetts Health Officers Association, Director, Town of Norwood Health Department
Laura Kittross, Western Massachusetts Public Health Association, Public Health Program Manager, Berkshire Regional Planning Commission
Robin Williams, President, Massachusetts Environmental Health Association, Environmental Health Manager, Framingham Department of Public Health
Carlene Pavlos, Executive Director , Massachusetts Public Health Association
MARCH 16, 2020
Question: Is school closure an effective mitigation for the COVID-19 outbreak?
Age-specific social distancing strategies for the COVID-19 outbreak
Marcia A. Testa, MPH, PhD 3/16/2020
In a recent Lancet article by Anderson et al. (March 6, 2020) entitled “How will country-based mitigation measures influence the course of the COVID-19 epidemic?” a number of mitigation efforts including school closures were discussed in the context of the COVID-19 outbreak. The effectiveness of non-pharmaceutical interventions such as school closures depend upon a number of factors, including the infectivity and severity rates in the schools and community. In the article, the authors state:
“A key issue for epidemiologists is helping policy makers decide the main objectives of mitigation—e.g., minimizing morbidity and associated mortality, avoiding an epidemic peak that overwhelms health-care services, keeping the effects on the economy within manageable levels, and flattening the epidemic curve to wait for vaccine development and manufacture on scale and antiviral drug therapies. ……School closure, a major pillar of the response to pandemic influenza A[1] is unlikely to be effective given the apparent low rate of infection among children, although data are scarce”.
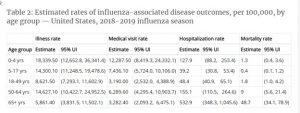
The rates of influenza per 100,000 show that the highest rate is in the age group 0 – 4 years 18,339.5 per 100,000 children aged 0 – 4 years, while the lowest rate is in those over 65 years, 5,861.5 per 100,000 (less than 1/3 the rate of children aged 0 – 4) However, the burden of illness as indicated by the hospitalization rate, is 4 times higher in those over 65 and with a mortality rate that is nearly 38 times higher (Table 2. From the CDC).
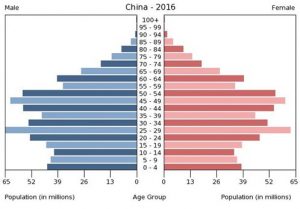
Unfortunately, there is no incidence data on the COVID-19 infection incidence rates by age from China since their data only contains the distribution of cases of individuals who tested positive among those who experienced symptoms and were brought to the attention of the medical facilities. However, the data from the Chinese CDC with 72,314 cases (Wu et al. , JAMA, 2/24/2020) strongly supports the low rate of symptomatic infection in younger individuals. The data from China, shows the number of cases by age group for the 44,672 confirmed cases of the 72,314 reported cases. One can get a very crude estimate of the relative incidence rates within the sample of diagnosed cases by using the age-specific frequencies of the general population data. (See graph below). Given the reported numbers in the Wu article and the population estimates in China, the positive COVID-19 infection rate in the < 20 age group was 14.5 x lower than that in the 30 – 79 age group.
To calculate the age distribution (N = 44 672) of confirmed cases in China, let us assume an age distribution similar to China as a whole. Assume a population in Wuhan of 11.2 million, Hubei province = 59 million, China = 1.4 billion. The population estimates are given in red. If one uses all of China, or Hubei Province or only the city of Wuhan, China in the denominator at risk the incidence rates of course will change, but the relative rates across the ages will remain the same.
- 80 year and older: 3% (1408 cases) per 100,000 7.8 cases– China, 185 cases – Hubei, 978 cases Wuhan
- 30-79 years: 87% (38 680 cases) or 7,736 per 10 year-age group. per 100,000 4.8 cases – China, 113 cases Hubei, 559 cases Wuhan
- 20-29 years: 8%(3619 cases) per 100,000 1.6 cases China, 37 cases Hubei, 198 cases Wuhan
- 10-19 years: 1% (549 cases) per 100,00 0.33 cases China, 7.8 cases Hubei, 41 cases Wuhan
- <10 years: 1% (416 cases) per 100,000 0.25 cases China, 5.9 cases Hubei, 31 cases Wuhan.
These data tell us that individuals less than 25 years of age have a very low incidence among those who sought medical care and who were subsequently diagnosed. With an influenza illness rates nearly 33,000 per 100,000 of 17 years and younger in the US, if one attributes all of the confirmed cases to Wuhan the rates are 71 per 100,000 for those 19 and younger. That is a rate for influenza in the US that is 464 times higher than COVID-19 in Wuhan.
What these data do not tell use is how many individuals with the virus were asymptomatic. There are only two possibilities, namely, 1) young children and adolescents are carriers of the virus with no or very mild symptoms, or 2) they are not infected. Denominator data are needed to determine the infection rates for the entire population at risk, independent of whether or not they presented at a health care facility.
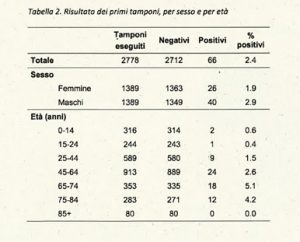
One population-based epidemiologic study in a village in northern Italy surveyed all residents in the town regardless of whether they had symptoms or not. Their data support a low rate of infection in children regardless of symptoms. Since the data did not select those that were tested based upon presenting to a health care facility with symptoms, these data provide evidence as to the actual infection rates in individuals with and without symptoms. This epidemiological study is being carried out in Vò , by Prof. Andrea Crisianti from the University of Padua. Vò is a comune in the Province of Padua in the Italian Veneto region, located about 50 kilometers west of Venice and about 20 kilometers southwest of Padua, in the western end of the Euganean Hills. Mount Venda forms part of its territory, at 603 metres the highest of the Hills area. As of 31 December 2018, it had a population of 3,341 and an area of 20.4 square kilometres. Vò became the center of the 2019–20 coronavirus outbreak in Veneto when two people were found positive on 21 February 2020. The next day, one of them, a 78-year-old man, died. This was the first death due to the virus in Italy. The number of infections had also risen to 29[1]. As of 28 February, there were 151 confirmed cases in Veneto, of which 70 cases in the municipality of Vò alone.[2]
Below is the survey data from Dr. Andrea Crisianti which shows the numbers of individuals in each age group that tested positive. Over 80% of the entire town was tested so one can make a fairly good assumption that this is a population-based sample. As seen here the average infection rate among all individuals under 25 years of age was 8.8 x lower (0.54%) as compared to those in the over 65 years of age group (4.74%).
The most useful data here is the low COVID-19 incidence rates among those younger than 25 in from China where individuals had symptoms or contacts to present for testing. Also important is the confirmatory the low infection rates in Vo for the population as a whole. In comparison to influenza, COVID-19 shows extremely low infections for adolescents and children, especially in the youngest ages.
Similar to influenza, COVID-19 has a much higher morality in the older ages. However, the infections rate is much higher in older ages than in children which is the inverse of influenza. Due to the very different demographic pattern, new types of social distancing migration efforts should be considered. For example, isolating the high-risk population with a great deal of focused social, psychological, and physical support, while allowing younger individuals to carry out their activities as usual – even supporting the older population, would result in an increase of mild or asymptomatic infections among the vast low risk population which is now estimated to be anywhere between 98 and 99%. However, this would allow them to acquire immunities naturally and eventually provide for herd immunity among the most vulnerable.
[1] Cauchemez S, Ferguson NM, Wachtel C, et al. Closure of schools during an influenza pandemic. Lancet Infect Dis 2009; 9: 473–81.
[1] “Coronavirus, ora sono 42 i contagiati veneti. Il focolaio resta Vo'”. Corriere Del Veneto.
[2] “Coronavirus, ora sono 42 i contagiati veneti. Il focolaio resta Vo'”. Corriere Del Veneto.
FEBRUARY 8, 2020
Coronavirus death toll hits 811, eclipsing SARS
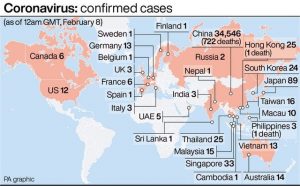
The death toll in China from the coronavirus has risen to 811, surpassing SARS fatalities in the 2002-2003 outbreak, Chinese health authorities announced on Sunday, 2/9/2020 China’s National Health Commission said total cases in the country from the virus had increased to to 37,198, up from 31,774 a day earlier. The outbreak of SARS, or severe acute respiratory syndrome, killed 774 people and infected more than 8,000 worldwide. Like the new virus, it also originated in China.
ARCHIVED
Man returning from Wuhan, China is first case of 2019 Novel Coronavirus confirmed in Massachusetts – Click to go to mass.gov news release
The Centers for Disease Control and Prevention (CDC) is closely monitoring an outbreak of respiratory illness caused by a novel (new) coronavirus first identified in Wuhan, Hubei Province, China. Chinese authorities identified the new coronavirus, which has resulted in hundreds of confirmed cases in China, including cases outside Wuhan, with additional cases being identified in a growing number of countries internationally. The first case in the United States was announced on January 21, 2020. There are ongoing investigations to learn more.
JANUARY 18, 2020 – CDC begins ‘enhanced’ health screenings at 3 airports due to China virus
Enhanced health screenings are being undertaken at three airports in the United States by the Centers for Disease Control and Prevention and the Department of Homeland Security’s Customs and Border Protection as a result of an outbreak of respiratory infections from a new coronavirus in the city of Wuhan in China’s Hubei Province.
The CDC and CBP began screenings Jan. 17 at San Francisco (SFO), New York (JFK), and Los Angeles (LAX) airports to detect ill travelers to this country on direct or connecting flights from Wuhan in response to an outbreak there caused by a novel coronavirus (2019 nCoV) that has resulted in 40 confirmed infections and two deaths in humans from the virus whose origin is being investigated in that city in Central China. To read full story, go to https://www.masslive.com/news/2020/01/cdc-begins-enhanced-health-screenings-at-3-airports-due-to-china-virus.html